Neutrophilic dermatoses are a group of heterogeneous disorders characterised by the infiltration of non-infectious neutrophils in the skin, with diverse cutaneous features (e.g., nodules, pustules, bulla, erosions, ulcerations) and extracutaneous symptoms.1 Common systemic findings such as fever, elevated inflammatory markers, inflammatory bowel disease and/or osteoarticular involvement suggest possible common pathogenic links (Figure 1).2 The mechanisms underlying neutrophilic dermatoses are not fully understood, but they may be viewed as a spectrum of autoinflammatory disorders, with several gene alterations identified and a central role for the interleukin-1 (IL-1) pathway.
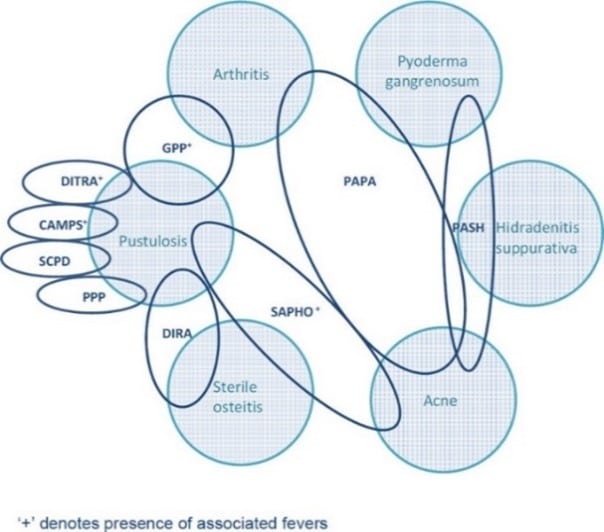
Figure 1. Overlapping features of pustular dermatoses. (From Naik HB, Cowen EW. Dermatol Clin. 2013 Jul;31(3):405-25.)
CAMPS, CARD 14-mediated pustular psoriasis; DIRA, deficiency of IL-1 receptor antagonist; DITRA, deficiency of the IL-36 receptor antagonist; GPP, generalized pustular psoriasis; PAPA, pyogenic arthritis, pyoderma gangrenosum, and acne; PASH, pyoderma, acne and suppurative hidradenitis; PPP, palmoplantar pustulosis; SAPHO, synovitis, acne, pustulosis, hyperostosis and osteitis; SPD, subcorneal pustular dermatosis.2
Generalised pustular psoriasis (GPP) is one epidermal neutrophilic dermatosis that is, although rare, can be severe and life threatening. It is critical to recognise GPP among other pustular psoriasis so as not to delay initiation of therapy.
References: 1. Salem I, Kimak M, Conic R, et al. Neutrophilic dermatoses and their implication in pathophysiology of asthma and other respiratory comorbidities: a narrative review. Biomed Res Int. 2019 Jun 10;2019:7315274. 2. Naik HB, Cowen EW. Autoinflammatory pustular neutrophilic diseases. Dermatol Clin. 2013 Jul;31(3):405-25.
COMPASS – Neutrophilic dermatoses: an overview
How much do you know about neutrophilic dermatoses? Learn to differentiate these autoinflammatory skin disorders with this course for a quick overview.
COMPASS – Generalised pustular psoriasis
Learn about the clinical presentation, clinical course and clinicopathologic considerations in diagnosing and available treatment options for GPP.